Dr. Jennifer Pearlman, MD CCFP NCMP FAARM ABAARM CFA
The new science of aging is rapidly expanding. Longevity experts predict that we will have the tools to achieve human immortality within our lifetime. By harnessing the retained ability of our tissues to repair and regenerate, longevity factors are being developed to reprogram aged tissues to a more youthful version of itself. Aging is no longer considered inevitable but rather a system problem that can be reprogrammed like out-of-date software.
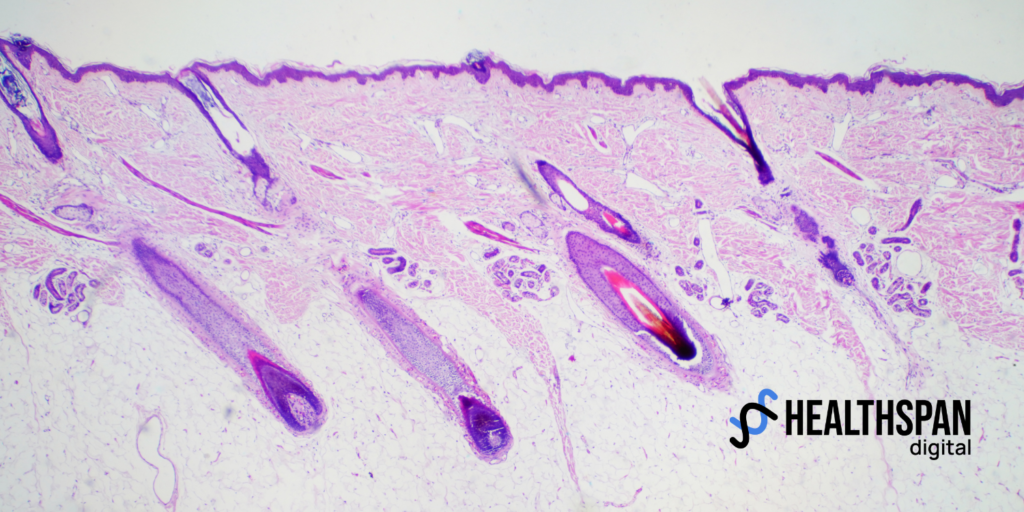
The goal of all this scientific progress is to live longer younger. If the added years of life were filled with disability, dysfunction and disease it would not be a worthy goal. Instead, extending lifespan to live with youth vitality and productivity is the essence of a longer healthspan. To age well requires that we first understand why we age. To date, a dozen hallmarks of aging have been identified. These root causes include; genomic instability, epigenetic drift, dysregulated nutrient sensing, inflammation, cellular senescence, stem cell depletion, telomere shrinkage and mitochondrial decline. Indeed, aging is very much a multi-system software failure. A pathological process that is best prevented rather than cured.
By the third decade of life, biological aging deviates from the rate of our chronological age. Furthermore, aging is tissue specific and age acceleration differs between women and men. The hallmarks of aging affect women differently than men just as there are gender differences in the diagnosis, treatment and prognosis of disease. Furthermore, midlife hormonal senescence specifically the dramatic decline of estrogen at menopause is a critical trigger to age acceleration in women.
Several biological aging clocks have been developed using biomarkers like telomere length and DNA methylation patterns to predict epigenetic age. Epigenetic clocks can predict fertility, age of menopause and correlate with other longevity markers.
For women, the midlife menopause transition is a time of rapid age acceleration during which DNA methylation decreases, genomic instability increases and telomere length shrinks. Nearly all of the hallmarks of aging are induced. The decade that saddles the final menstrual cycle represents the most rapid aging of a women’s lifespan, three times faster than any other and twice as fast as men who also experience more rapid aging in their midlife. The loss of ovarian estrogen release is a major factor to this rapid aging as estrogen upholds the entire longevity apparatus.
Estrogen has direct effects on genomic expression, telomeres, mitochondrial function and immunity. With estrogen receptors throughout the body and brain, the effects of menopausal estrogen loss are widespread. The most common symptoms of menopause relate predominantly to the brain with hot flashes, night sweats, sleep and mood disturbances as typical concerns. But menopause’s effects are also widespread and more innocuous with a significant increase in the risk of chronic diseases of aging including heart disease, diabetes, dementia and osteoporosis. Women who experience menopause early, before the age of 45 years have a 12% shorter average lifespan than those who reach menopause after the age of 53.
Hormonal optimization therapy (HOT) refers to a proactive personalized approach to manage hormones throughout our lifespan and particularly in the midlife transition. There are hundreds of circulating hormones and all must be balanced much like a symphony orchestra to achieve optimal health and vitality. Combined estrogen and progesterone therapy using bioidentical individualized treatment plans can alleviate troublesome menopausal symptoms and mitigate disease risk. But there is a window of opportunity, as the risk-benefit ratio of hormone therapy is most favourable in the years immediately following the last menstruation. For women in their late postmenopausal years who have not yet initiated hormone therapy, the risk of systemic estrogen may outweigh the potential benefit.
While hormones play a vital role throughout the lifespan to our health outcomes and disease risks, they are just one piece of the aging puzzle. A comprehensive longevity approach must consider the hallmarks of aging and an individual’s unique needs and goals.
Women are born with a set of biologic longevity advantages but also unique susceptibilities. Midlife hormonal changes underlie both health and aging risks. The menopause related decline in estrogen results in accelerated aging as estrogen is geroprotective. Optimizing hormones and expertly managing the menopause transition can offset the age acceleration otherwise experienced at this time. Estrogen is an important longevity factor and for midlife women can be key to healthy aging.
Dr. Pearlman is a visionary health entrepreneur and an internationally recognized medical expert in health, hormones and regenerative medicine. She is a medical director and owner of PearlMD in Toronto, Canada where she offers customized solutions to help women live longer younger. She is a staff physician at Mount Sinai Hospital in Toronto where she helped lead the menopause clinic, the largest of its kind in Canada. Dr. Pearlman is a NAMS certified menopause expert, fellow and faculty of An5-Aging and Regenerative Medicine by A4M, Director of Regenerative Aesthetics with AMWC. Dr. Pearlman is co-founder and Director of Business Development for Healthspan Digital offering a first in class AI powered longevity platform as an enterprise solution.